Knowing who shouldn’t get dental implants helps patients avoid needless procedures, complications, and wasted money. Dental implants work great to replace missing teeth, but they’re not right for everyone.
Patients should know several key factors determine if they can get implants. Your dentist will need a detailed health history to assess whether you’re a good candidate for dental implants. Sufficient jawbone density plays a crucial role in successful implant placement. Some health conditions can substantially affect how well you heal after implant surgery – these include uncontrolled diabetes and autoimmune disorders. Heavy smoking makes healing harder and raises your risk of implant failure.
This piece gets into the key factors that might rule out dental implants as an option. We’ll help you make smart choices about ways to restore your oral health.
Jawbone and Bone Density Issues
Your jawbone creates the foundation for successful dental implant treatment. The density of your bone plays a crucial role in determining if dental implants will work for you.
Why bone health matters for implants
Dental implants work as artificial tooth roots that must fuse with your jawbone through a process called osseointegration. This biological bond needs enough quality bone to support the implant effectively. Dentists assess bone density because it relates directly to bone strength and stability.
Chewing creates mechanical stress that affects the area where bone meets the implant. Higher bone density helps distribute this stress better and gives the implant stronger long-term support. Research shows that implants placed in poor quality bone have substantially lower survival rates.
What happens if you have bone loss?
Your body naturally loses bone mass after losing teeth. The jawbone can lose up to 25% of its width during the first year without tooth root stimulation. This bone loss keeps going and might reach 80% of bone height over three years.
Your jawbone must be at least 3mm wide and 10mm high to support an implant. Lower bone density reduces the implant’s stability and might lead to failure. Doctors don’t recommend placing implants in D4 bone (very low density) because failure rates range from 35-50%.
Bone grafting as a possible solution
Bone grafting gives hope to patients who don’t have enough bone density. This surgery rebuilds or increases bone mass by adding material that becomes part of your natural bone.
You have several grafting options:
- Autograft: Bone from another location in your body
- Allograft: Bone from a human donor
- Xenograft: Bone from an animal source
- Synthetic: Bone-substitute materials
About half of all dental implant surgeries need bone grafting. The implant needs to be placed within 6-12 months after a successful graft. The grafted bone starts to shrink and lose density if not used during this time.
Dentists use different grafting methods to fix specific bone problems, including ridge preservation, tunnel grafts, block grafts, and sinus lifts.
Oral Health Conditions That Disqualify You
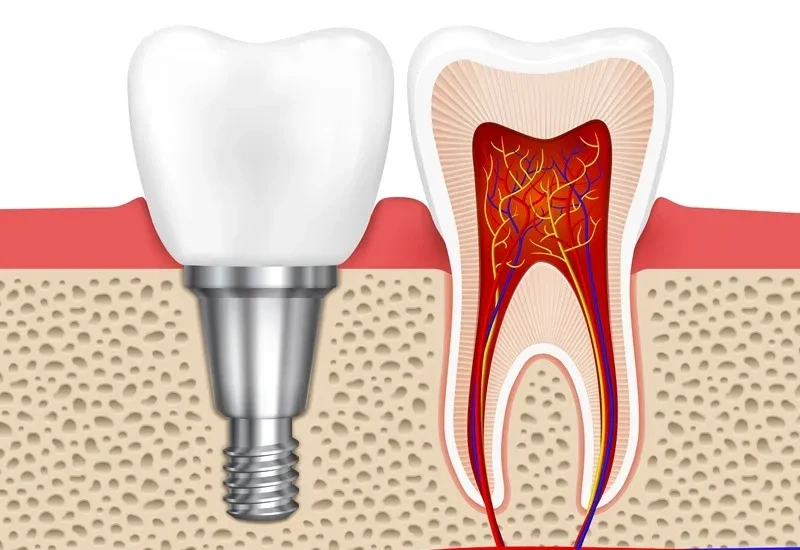
Image Source: Advanced Dental Concepts of Oakland
Oral Health Conditions That Disqualify You
Healthy oral tissues are the life-blood of successful dental implant treatment. Your bone structure might be adequate, but certain oral health conditions can still make you unsuitable for dental implants.
Untreated gum disease
Periodontal disease damages gum tissue and bone through a serious bacterial infection. The condition progresses through these stages:
- Gingivitis – original inflammation with bleeding gums
- Periodontitis – gums pull away from teeth and form infected pockets
- Advanced periodontitis – bone and tissue face massive destruction
Research shows gum disease causes most adult tooth loss. We focused on treating active periodontal problems first because infection weakens the foundation implants need. Bacteria can spread to implant sites and compromise osseointegration, which leads to early failure.
Chronic oral infections
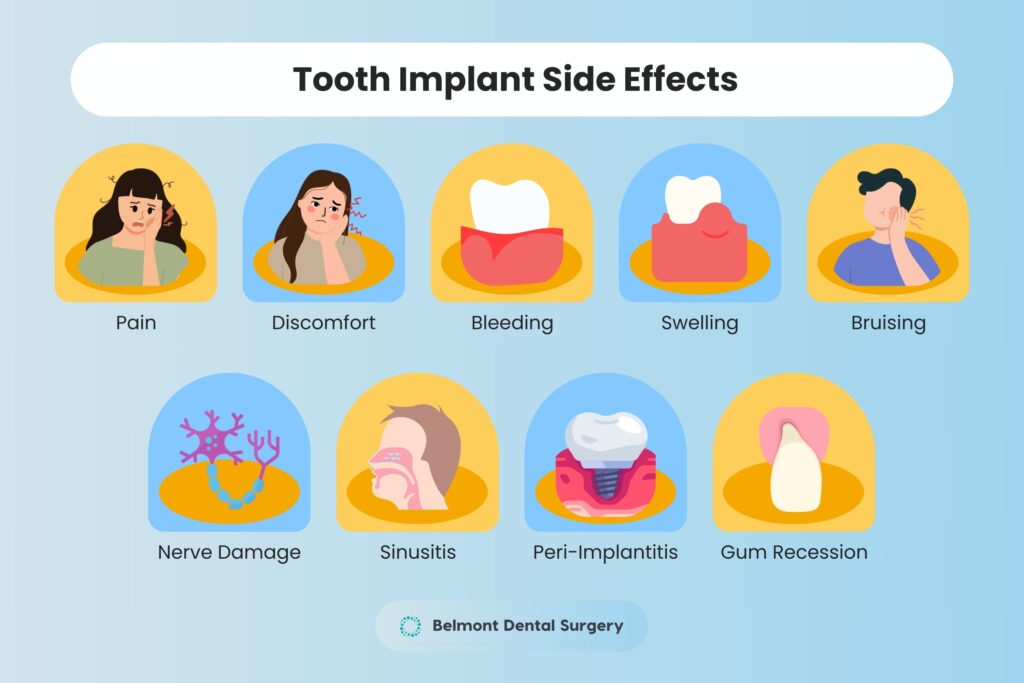
Dental implants cannot heal properly in a mouth with untreated infections. Peri-implantitis, an infection like gum disease that affects implant’s surrounding tissues, creates a major risk to stability.
These infections start with inflammation and discomfort. The bone around implant sites deteriorates over time. The bacteria can enter your bloodstream and make heart disease and diabetes worse.
Poor oral hygiene habits
Studies show 56.4% of implants succeeded in patients with poor oral hygiene. The disease rates soared especially when patients had visible plaque/calculus and didn’t brush enough.
Watch for these implant problem signs:
- Red, swollen, or bleeding gums around the implant
- Bad breath that won’t go away or unpleasant taste
- Gum recession showing more implant
- Pain during chewing
Dental experts recommend thorough oral hygiene with regular brushing, flossing, and professional cleanings to protect implants’ success. Patients who don’t show steadfast dedication to oral care rarely qualify as good candidates for dental implants.
Medical Conditions That May Prevent Implant Success

Image Source: Wiley Online Library
Medical Conditions That May Prevent Implant Success
Medical conditions throughout the body affect dental implant success rates. These conditions can hurt the healing process needed for successful osseointegration.
Uncontrolled diabetes
Patients who can’t control their diabetes have much higher implant failure rates[link_1]. High blood sugar levels stop osteoblastic activity, reduce collagen formation, and kill bone lining cells. Diabetic patients with good control can achieve success rates similar to non-diabetics. However, uncontrolled diabetics face poor healing and higher infection risks. Diabetes causes small blood vessel problems that directly hurt osseointegration.
Autoimmune disorders
Conditions like Sjögren’s syndrome, rheumatoid arthritis, and lupus can affect implant success through changed inflammatory responses. The immune system attacks the body’s tissues in these conditions and complicates healing after implant surgery. Research shows implant survival rates in autoimmune patients match the general population when patients keep excellent oral hygiene.
Blood clotting issues
Blood disorders come in three types: congenital coagulation disorders, antiplatelet-induced bleeding disorders, and anticoagulant-induced bleeding disorders. Doctors must evaluate these conditions carefully before surgery and follow special protocols. Patients with bleeding problems can get implants safely but need modified surgical approaches and extra post-surgery care.
Impact of certain medications
Some medications can hurt implant outcomes. Bisphosphonates used to treat osteoporosis can cause jaw bone death. Studies show SSRIs boost implant failure by about 7.5% [link_2]. PPIs used for acid reflux raise failure rates by 4.3% because they block calcium absorption.
Lifestyle Habits That Can Interfere with Healing
Image Source: Antlara Dental Clinic
Lifestyle Habits That Can Affect Healing
Your lifestyle choices can affect dental implant success by a lot, even with favorable clinical conditions. These habits directly affect how implants bond with bone and stay stable long-term.
Smoking and tobacco use
Tobacco use stands out as one of the biggest risks for implant failure among patients. Studies show failure rates in smokers range from 6.5% to 20% compared to non-smokers. Nicotine shrinks blood vessels and reduces blood flow to oral tissues, which makes healing harder. Smokers lose more bone around their implants after placement. The data shows implants fail 2.4 times more often in smokers than non-smokers.
Alcohol abuse
Too much alcohol hurts implant success in several ways. Heavy drinkers develop 46.2% rate of peri-implantitis while light-to-moderate drinkers only show 11.5%. A small amount of alcohol actually helped reduce late implant failure by 75%. But heavy drinking makes peri-implantitis almost three times more likely.
Teeth grinding (bruxism)
Bruxism puts too much pressure on implants through grinding and clenching. Common problems include:
- Porcelain fracture
- Screw loosening
- Decementation
- Poor bone integration
People who grind their teeth face 2.18 times higher risk of implant failure than those who don’t.
Neglecting follow-up care
Dentists need regular check-ups to catch problems early. Missing appointments means they can’t fix issues like infections or misalignment quickly enough.
Conclusion
Dental implants can change people’s lives, but several key factors determine if someone can get this treatment. A patient’s jawbone density is the foundation of successful implants. Without enough bone, the implants won’t integrate properly. The good news is bone grafting helps many patients who don’t have enough bone density, though this adds time to the treatment.
Good oral health is the life-blood of implant success. Untreated gum disease, ongoing infections, and poor dental habits lead to higher failure rates. These issues need treatment before a patient can move forward with implants.
A patient’s overall health plays a big role in how well implants work. People with uncontrolled diabetes don’t heal well, and autoimmune conditions can make recovery harder. Blood disorders and some medications need special attention before any implant surgery.
The way people live their lives affects implant success too. Smoking makes implants fail more often, and too much alcohol raises the risk of implant infections. Teeth grinding puts too much pressure on implants and makes them unstable. Following post-surgery care instructions is also vital.
No one should decide on their own if they can get dental implants. A complete evaluation by qualified dentists helps spot risks and create the right treatment plan. Many people who don’t qualify at first can become good candidates with the right preparation. This might mean bone grafting, gum treatment, changing medications, or lifestyle changes.
Dental implants are amazing at restoring teeth, but they’re not right for everyone. Good screening and preparation help ensure success and avoid problems. Patients should have realistic expectations and understand their personal risk factors well.
FAQs
Q1. Who are not suitable candidates for dental implants? Individuals with insufficient jawbone density, untreated gum disease, uncontrolled diabetes, certain autoimmune disorders, or those who smoke heavily may not be suitable candidates for dental implants. A comprehensive evaluation by a dental professional is necessary to determine eligibility.
Q2. What are the potential risks associated with dental implants? Risks include implant failure due to poor osseointegration, infection, nerve damage, and sinus problems. Additionally, lifestyle factors like smoking or teeth grinding can compromise implant success. Regular follow-up care is crucial to mitigate these risks.
Q3. Can bone grafting make someone eligible for dental implants? Yes, bone grafting can often make patients with insufficient bone density eligible for implants. This procedure rebuilds or augments areas lacking adequate natural bone, providing a foundation for successful implant placement. However, it may extend the overall treatment timeline.
Q4. How do certain medications affect dental implant success? Some medications, such as bisphosphonates for osteoporosis, selective serotonin reuptake inhibitors (SSRIs), and proton pump inhibitors (PPIs), can negatively impact implant outcomes. These medications may increase the risk of implant failure or complications, necessitating careful consideration and potential adjustments to treatment plans.
Q5. What role does oral hygiene play in dental implant success? Maintaining excellent oral hygiene is crucial for dental implant success. Poor oral hygiene habits can lead to infections, inflammation, and eventual implant failure. Regular brushing, flossing, and professional cleanings are essential to protect the long-term viability of dental implants.